M&D Clinical Corner: Community Pharmacist’s Guide to Continuous Glucose Monitoring
The Clinical Corner is a monthly feature that highlights a variety of important pharmacist topics that is written by Morris & Dickson’s staff pharmacist, Paula Belle (RPh).
This month’s Clinical Corner will discuss continuous glucose monitoring (CGM):
- Facts and Figures
- The Role of the Pharmacist
- Advantages of CGM
- Examples of Available CGM
- Examples of CGM Parts and Methods of Operation
- Resources for Pharmacists
- Resources for Patients
Facts and Figures
- Finger stick blood sugar testing daily or multiple times a day (depending on the type of diabetes) was a standard of care for diabetic patients since the early 80’s. [1]
- The scientific community knew a fingerstick glucose reading represented only a point in time and did not tell the whole story of blood glucose levels. [1]
- Continuous glucose monitoring or CGM continuously monitors blood glucose, providing real-time updates through a device that is attached to the patient’s body. [2]
- CGM has become popular and more accurate over the years and is now considered a viable treatment option for people with diabetes. [2]
- By 2016, the accuracy of these sensors was so good that the U.S. Food and Drug Administration (FDA) approved continuous glucose readings to replace fingerstick blood sugar testing altogether. [1]
- Effective April 16, 2023, the Centers for Medicare and Medicaid Services (CMS) expanded CGM coverage to include a broader group of Type 2 diabetics using insulin as well as certain non-insulin-using individuals who have a history of “problematic hypoglycemia.” [3]
- The expanded coverage approved by CMS is expected to increase access to CGM for approximately 1.5 million people with diabetes. [3]
- Monitors used in CGM are small devices worn on the body, typically on the abdomen or back of the arm, that monitor the interstitial glucose every 1 to 5 minutes. [1]
- With CGM, people living with diabetes are always aware of their blood sugar levels. [1]
The Role of the Pharmacist
- CGM is an opportunity for pharmacists to use their skills to improve a patient’s quality of life and health management. [4]
- Pharmacists can be at the forefront of initiating a patient on CGM by identifying patients and helping them to eliminate initial barriers. [4]
- Any of the following may be an indication for personal CGM for patients with Type 1 or Type 2 Diabetes [5]:
- Taking multiple daily injections of insulin
- Using an insulin pump
- Frequent hypoglycemia
- Hypoglycemia unawareness
- High degree of glycemic variability
- Not achieving glucose targets
- The use of technology should be individualized based on a patient’s needs, desires, skill level, and availability of devices . [5]
- One of the largest reasons diabetic patients do not get the devices they need is cost. [6]
- Pharmacists can determine which insurance plans cover CGM by utilizing this link: https://www.diabeteseducator.org/danatech/glucose-monitoring/continuous-glucose- monitors-(cgm)/cgm-insurance-coverage-look-up
- Pharmacists can research programs that can assist patients with no insurance or those that are underinsured at this link: https://www.diabeteseducator.org/danatech/glucose- monitoring/continuous-glucose-monitors-(cgm)/cgm-affordability-programs
Pharmacists can assist patients in understanding the general differences in CGM devices. [7]
*These represent some available CGM systems and do not include all makes and models of CGM devices.
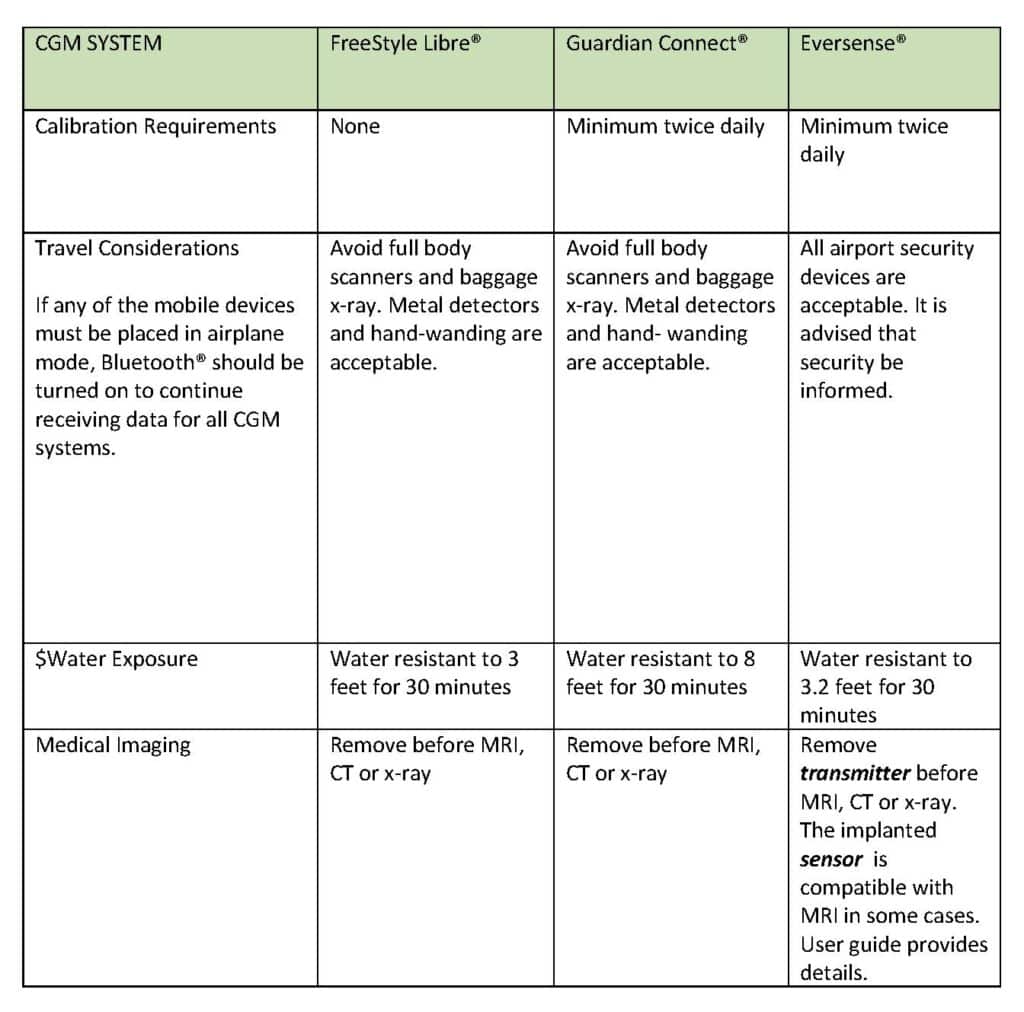
Source: Therapeutic Research Center, Continuous Glucose Monitoring. May 2023: Pharmacist’s Letter
Pharmacist may also provide tips for success with CGM. [7]
- They can advise patients that some CGM model sensors are placed on the back of the arm and other brands have sensors that should be placed on the abdomen. [8]
- The selected application site should be cleansed with non-moisturizing, fragrance-free soap and water. [8]
- The skin should then be dried after cleansing and wiped with an alcohol wipe and allowed to dry prior to placing the sensor. [8]
- When placing the sensor, patients should avoid scars, moles, lumps, irritated skin, stretch marks, insulin injection sites, and the navel. [8]
- To improve adhesion, patients should avoid placing sensors on the waistline or beltline, in hairy areas, areas where there is movement or bending, areas where clothing may rub or areas where the sensor may dislodge when asleep. [8]
- When patients experience issues with sensors that do not stay on, pharmacists can recommend products to improve adhesion such as Skin Tac® or Tegaderm®. [7] However, pharmacists should advise patients to check the instructions for their CGM sensor as some parts may be required to remain uncovered. [8]
- Some sensors, such as those used with the Freestyle Libre®, should not be reattached if they fall off. [8]
- Patients should be advised to be cautious with doorways, car doors, seat belts, and furniture edges to prevent accidental dislodging of the CGM sensor. [8]
- Pharmacists can recommend that patients wear clothing that fits loosely in areas that contact the CGM sensor. [8]
- Pharmacists can advise patients that, depending on the brand, some CGM systems may take from ½ hour to up to 24 hours after application to provide glucose readings. [8]
- Most sensors are removed similar to removing a bandage, by peeling from the edge. [8]
- Some CGM systems (Guardian 3®) have reusable transmitters attached to the sensors and these should be removed prior to removing the sensors. [8]
- Once removed, sensors should be disposed of in containers that are appropriate for sharps and blood exposure. [8]
- Pharmacists can recommend baby oil or adhesive remover for patients who have difficulty removing all of the sensor adhesive from their skin. [8]
- Pharmacists should advise patients to rotate sites when applying their next CGM sensor. [8]
- Advantages of CGM
- CGM can measure blood glucose every few minutes to show how blood glucose levels change over time and reveal the bigger picture of how diabetes affects a patient. [9]
- Using CGM to monitor blood glucose over time can help patients and their providers understand how things like food, activity, stress, and illness impact glucose levels. [9]
- Providers can review data from CGM for patterns and trends and can then individualize care for the patient. [9]
- Alarms can be set to alert the person to these events so they can make informed decisions. An example alert might be set to indicate if the person’s blood sugar hits 70 mg/dL or less via an alarm that goes off so that the person knows to eat or drink a small amount of sugar before they drop any lower. [1]
- The need for fingerstick checks will not be eliminated because fingerstick checks measure glucose levels in blood and provide the best picture of what the glucose level is at the precise moment of the stick. CGM measures glucose under the skin, which shows where glucose levels were five to 10 minutes ago. The use of a CGM can significantly reduce the number of fingerstick tests that a patient requires each day. [9]
- Available CGM System Examples
- Professional CGM System Examples
- These systems may be available via the patient’s provider for short-term use to analyze trends and include makes and models such as Freestyle Libre Pro® and iPro2 Professional ®. [8]
- Personal CGM System Examples
- These CGM systems are used long-term by the patient for diabetes management and include stand-alone monitors as well as integrated models that integrate with insulin pump technology. [8]
Advantages of CGM
- CGM can measure blood glucose every few minutes to show how blood glucose levels change over time and reveal the bigger picture of how diabetes affects a patient. [9]
- Using CGM to monitor blood glucose over time can help patients and their providers understand how things like food, activity, stress, and illness impact glucose levels. [9]
- Providers can review data from CGM for patterns and trends and can then individualize care for the patient. [9]
- Alarms can be set to alert the person to these events so they can make informed decisions. An example alert might be set to indicate if the person’s blood sugar hits 70 mg/dL or less via an alarm that goes off so that the person knows to eat or drink a small amount of sugar before they drop any lower. [1]
- The need for fingerstick checks will not be eliminated because fingerstick checks measure glucose levels in blood and provide the best picture of what the glucose level is at the precise moment of the stick. CGM measures glucose under the skin, which shows where glucose levels were five to 10 minutes ago. The use of a CGM can significantly reduce the number of fingerstick tests that a patient requires each day. [9]
Available CGM System Examples
Professional CGM System Examples
- These systems may be available via the patient’s provider for short-term use to analyze trends and include makes and models such as Freestyle Libre Pro® and iPro2 Professional ®. [8]
Personal CGM System Examples
- These CGM systems are used long-term by the patient for diabetes management and include stand-alone monitors as well as integrated models that integrate with insulin pump technology. [8]
Stand Alone CGM System Examples [8]
- Medtronic Guardian Collect® (compatible mobile devices available at: https://medtronicdiabetes.com/customer-support/guardian-connect-faqs )
- Senseonics Eversense ® (compatible mobile devices available at: https://ascensiadiabetes.com/eversense/compatability/ )
- Freestyle Libre 2®, Freestyle Libre 3®, Freestyle Libre 14 Day® (compatible mobile devices available at: https://freestyleserver.com/Payloads/IFU/2022/q4/ART41556- 202_rev-L-web.pdf )
Integrated CGM System Examples [8]
- Guardian Sensor 3® is compatible with Medtronic MiniMed 630G® and 770G® pumps.
Examples of CGM System Parts and Methods of Operation
Most CGM systems contain a sensor, transmitter and receiver. [6]
Sensor
- Sensors are inserted under the skin to measure blood glucose. [6]
- Sensors need to be changed and the interval varies by machine brand [8]:
- Guardian 3® – every 7 days.
- Freestyle Libre® Systems – every 14 days
- Eversense® – every 6 months.
Transmitter
- Transmitters may be reusable or disposable. [8]
- These attach to a sensor base and transmit glucose levels to the receiver or reader. [8]
- Transmitters must be within range of the receiver and this range can vary by machine brand [8]:
- Guardian Sensor 3® within 20 feet.
- Senseonics Eversense® within 24.9 feet.
- Freestyle Libre 3® within 33 feet
Receiver
- The receiver displays current and stored glucose readings. [8]
- Most CGM systems transmit data in real-time. [8]
- Most CGM systems will send data to a smartphone or dedicated reader. [8]
Resources for Pharmacists
- CGM Patient Candidate Assessment Website: https://www.diabeteseducator.org/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/cgm-selection-training/candidate-selection-characteristics-(cgm)
- CGM Device Assessment Website: https://diabeteswise.org/en/device-finder/all
- Find and Compare CGM: https://www.diabeteseducator.org/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/view-compare-cgms
- APhA: Personal Continuous Glucose Monitoring Implementation Playbook: https://aphanet.pharmacist.com/sites/default/files/files/PERSONAL%20CGM%20PLAYBOOK%20-%20FINAL%20VERSION%201-13-2021.pdf
- ADCES: The Role of Continuous Glucose Monitors (CGM) in Diabetes Management : https://www.diabeteseducator.org/docs/default-source/practice/educator-tools/role_cgm_12272021.pdf
- ADCES: Diabetes Technology Device and Programming Training: https://www.diabeteseducator.org/danatech/training-education/danatech-device-training
Resources for Patients
- ADCES: Pocket Guide Continuous Glucose Monitoring Connecting the Dots: https://www.diabeteseducator.org/docs/default-source/living-with-diabetes/guides/pocket_cgm_guide_english.pdf?sfvrsn=2
- ADCES Managing Blood Sugar with Time in Range: https://www.diabeteseducator.org/docs/default-source/practice/educator-tools/timeinrangetipsheet_2020.pdf?sfvrsn=2
- AAFP CGM Handout For Patients: AAFP Continuous Glucose Monitoring.pdf
Sources
- McKee, A.M.M. Continuous Glucose Monitoring (CGM): History, Benefits, Comparison of Models. 2023; Available from: https://www.endocrineweb.com/conditions/diabetes/continuous-glucose-monitoring.
- American Diabetes Association. CGM Support | ADA. 2023 [cited 2023; Available from: https://diabetes.org/get-involved/advocacy/continuous-glucose-monitors.
- Moreau, D. Final Medicare Continuous Glucose Monitor (CGM) Policy Goes into Effect April 16th. 2023; Available from: https://www.diabeteseducator.org/news/perspectives/adces-blog-details/danatech-latest-news/2023/04/07/final-medicare-continuous-glucose-monitor-(cgm)-policy-goes-into-effect-april-16th.
- Cook, K. and J. Ogurchak. Continuous Glucose Monitoring: An Opportunity to Understand and Individualize Diabetes Management. 2023 [cited 2023; Available from: https://www.pharmacytimes.com/view/continuous-glucose-monitoring-an-opportunity-to-understand-and-individualize-diabetes-management.
- Association of Diabetes Care and Education Specialists, American Pharmacists Association, and American Pharmacist Association Foundation, Personal Continuous Glucose Monitoring Implementation Playbook. 2020.
- Isaacs, D. CGM Affordability Programs. 2023 [cited 2023; Available from: https://www.diabeteseducator.org/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/cgm-affordability-programs.
- Therapeutic Research Center Healthcare, Answer FAQs About Continuous Glucose Monitoring. May 2023: The Pharmacist’s Letter.
- Therapeutic Research Center, Continuous Glucose Monitoring. May 2023: Pharmacist’s Letter.
- Cleveland Clinic. Continuous Glucose Monitoring (CGM): What Is It & How Does It Work. 2023 [cited 2023; Available from: https://my.clevelandclinic.org/health/drugs/11444-glucose-continuous-glucose-monitoring.